If you have experienced lower back pain you are not alone.Nearly 80 percent of adults have, or will have, suffered from it at some point in their lives. It’s the most common cause of job-related disability, a leading contributor to missed work days. Physical Therapists treat this diagnosis more frequently than any other. For that reason, we’re here to answer your questions, inform you, about the research and maybe even bust some myths. Did you know that Physical Therapy (PT) is one of the most economical, safe, and effective ways to treat most cases of lower back pain?
Should I see my doctor for lower back pain?
If your back pain started immediately after a fall, visit your doctor before starting physical therapy. Additionally, your insurance may require a referral for PT. If so, call or see your doctor to request a referral so we can bill your insurance.
Other than those instances, it’s more effective to see a physical therapist first. Usually, our findings are routine and point to a typical pattern of pain. In that case, we prescribe a home exercise program to do in conjunction with your physical therapy treatments. If we find a reason for you to see your doctor, we will tell you why. Finally, we always send your doctor a summary of the initial evaluation, progress report and discharge status.
I saw my doctor and all they did was refer me to physical therapy. Isn’t there anything else they can do?
Fist bump!! You’ve chosen a good doctor who’s read the research and knows the best place for you to start. Yes, doctors can prescribe medicines and order imaging, but increasingly, the research supports not doing this from the get-go.
Do I need prescription medications for lower back pain?
It’s important to note that there are no medications that fix lower back pain, only minimize symptoms. Unfortunately, all prescription drugs come with side-effects.
The most common medications prescribed for lower back pain are Nonsteroidal Anti-Inflammatory Drugs (NSAIDS) and muscle relaxants. NSAIDS can take the edge off. These come with the side effects of delayed tissue healing and an upset stomach. Muscle relaxants help during a gripping muscle spasm, but they make you drowsy. Therefore, most people can only take them at night.
Opioid pain-killers are highly addictive. For that reason, all conservative options should be exhausted before using opioid pain-killers for lower back pain.
Should I have imaging for lower back pain?
The short answer is NO. Unless you have red flags, imaging won’t provide information that will change the course of your treatment. Plus, it increases the over-all cost of treatment, exposes you to unnecessary radiation and might find things that you’ll feel bummed about the rest of your life (happens all the time!). For example, many people have degenerative changes in their spine but have no symptoms. As a result, finding something like this makes you worry and feel old or broken. What’s worse, it distracts you from the proactive steps you can take to get rid of the pain.
Imaging for lower back pain can be worse than useless because it can send you down a path of trying to fix something that may have nothing to do with the pain you’re experiencing. Unfortunately, patients are often the ones demanding imaging. In the absence of red flags, healthcare providers ordering imaging for lower back pain either aren’t current on the research or are caving to their patient’s demands.
How can we fix lower back pain if we don’t know exactly what’s wrong?
Humans are complex (and interesting). If we were robots we could run some diagnostics, write some code, switch out parts and be good as new. Back pain is a symptom that can get better even if we don’t know the exact cause. As a human, every—single—thing about you is unique. Your DNA, life experiences, daily activities, diet, exercise, posture, mental outlook, over-all health all feed into how you experience pain. A picture of your spine isn’t sophisticated enough to reveal all of your unique characteristics.
Which exercises, or activities should I avoid with lower back pain?
The only uniformly recommended treatment for lower back pain in the literature is exercise. However, it’s good to modify activities that increase pain. Ideally, the exercises your physical therapist prescribes should be pain-free or not increase your baseline level of pain. Sometimes, it isn’t the activity that’s the problem, but the way that you’re performing it. Physical therapists are experts at teaching correct posture, body mechanics and lifting mechanics.
What exercises or activities should I do for lower back pain?
Movement is the best medicine for lower back pain. However, we can’t say uniformly that all patients should participate in certain exercises. We commonly recommend yoga or Pilates to our patients, although the research isn’t conclusive. This is likely due to our uniqueness (once again). For example, people who have very loose joints could do more harm than good by practicing certain types of yoga.
Physical therapists are uniquely trained to examine anatomic and physiologic variations. Therefore, we’re distinctively qualified to recommend exercises and activities that work best for your body, lifestyle and preferences.
How long will the lower back pain last?
Generally, an acute episode of lower back pain can last up to 6 weeks. A sub-acute episode is one lasting 6-12 weeks, and chronic lower back pain lasts more than 12 weeks.
Will lower back pain come back?
Estimates of having a recurrence in the first year after an episode up to 80%. Don’t get discouraged just yet because here’s what we see. Patients who actively participate in therapy (do their home exercise program; change daily habits; reach all their activity goals) are much less likely to experience a recurrence.
Those that see healthcare as a passive experience (i.e. you fix me) tend to experience higher rates of recurrence. Similarly, patients often stop therapy after getting pain-relief from a few sessions of PT. Unfortunately, the problem hasn’t magically gone away. Odds are the pain will return within the year.
What are these red flags for lower back pain?
Red flags are symptoms that require a visit to your doctor who can order the appropriate tests.
Red Flags:
- Recent fall
- Fever
- Saddle anesthesia (numbness or tingling in the perineum)
- Sudden bowel or bladder changes
- Progressive weakness over a short period of time (e.g. I could move my big toe yesterday, but today I can’t)
As you see, physical therapy should be your first line of defense for the treatment of low back pain. Call us, or CLICK HERE, to schedule your first appointment!
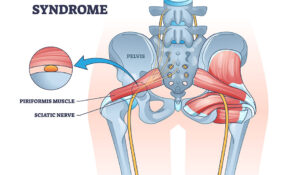
- Sciatica or Piriformis Syndrome? 3 Ways to Tell the Difference (Self-Test Guide) - December 22, 2025
- What Is Gout? Why It Happens and What You Can Do About It - November 17, 2025
- 3 Essential Back-Saving Tips You MUST Know Before Any Workout - November 14, 2025